What is a Thyroid Nodule?
Thyroid nodule refers to thyroid cells that show abnormal growth and form a lump within the thyroid gland. Thyroid nodules are detected in 5-6% of physical exams and 20-45% of ultrasound examinations. The frequency of thyroid nodules increases after the age of 50. About 95% of these nodules are benign (non-cancerous), while 5% may contain malignant (cancerous) cells.
What causes thyroid nodules?
Thyroid nodules can occur due to the following reasons:
- Iodine deficiency
- History of radiation exposure to the neck area
- Family history of thyroid nodules or thyroid cancer
- Iron deficiency anemia
- Smoking
- Obesity
- Presence of metabolic syndrome
- Insulin-like growth factor 1 (IGF-1)
- Thyroid nodules are 6-7 times more common in women than in men.
- The frequency of thyroid nodule development increases after the age of 50.
What are the types of thyroid nodules?
The types and characteristics of thyroid nodules are as follows:
- Colloid nodules: The most common type of thyroid nodule. It is an excessive growth of normal thyroid tissue. These nodules have no risk of cancer.
- Cystic nodules: Nodules filled with fluid. Cystic nodules pose a low risk for cancer. Nodules larger than 2 cm are monitored by ultrasound, or thyroid biopsy is performed.
- Semisolid nodules: These nodules contain both fluid and solid (hard) components. If there is suspicious appearance in the solid part of the nodule during ultrasound, a biopsy may be performed.
- Inflammatory nodules: These nodules develop as a result of chronic inflammation of the thyroid gland (thyroiditis). In the flare-up phase of thyroiditis, they may cause pain in the patient.
- Multinodular goiter: In multinodular goiter, there are multiple thyroid nodules causing enlargement of the thyroid gland.
- Hyperfunctioning thyroid nodules (Hot nodules): These nodules produce more thyroid hormone than normal. As a result, the patient develops hyperthyroidism symptoms.
- Nonfunctioning thyroid nodules (Cold nodules): These nodules do not produce thyroid hormones and do not change the TSH levels in the blood.
- Thyroid cancer: Thyroid cancer is found in less than 5-6% of all thyroid nodules.
What are the symptoms of thyroid nodules?
The symptoms of thyroid nodules include:
- Lumps visible on the neck or palpable during a physical examination in large and superficially located nodules.
- Difficulty swallowing due to compression of the esophagus by the thyroid nodule.
- Breathing difficulties due to compression of the trachea by the thyroid nodule.
- Hoarseness or voice changes caused by compression of the vocal cords by the thyroid nodule.
- If the thyroid nodule is hyperactive (hot nodule), it secretes excessive thyroid hormones, leading to symptoms of hyperthyroidism (heart palpitations, tremors, high blood pressure, weight loss, hot flashes, etc.).
Conditions where thyroid nodules are more likely to be cancerous
- In thyroid ultrasound, nodules with significant hypoechoic areas, microcalcifications, irregular borders, or when the height is greater than the width.
- Rapid increase in the size of the thyroid nodule (more than 20% increase per year).
- Involvement of thyroid nodules extending beyond the thyroid to surrounding structures (such as the trachea and lymph nodes).
- Hoarseness or thickening of the voice (indicating involvement of the vocal cord nerve).
- Presence of suspicious lymph nodes indicating metastasis during thyroid ultrasound examination.
- Age under 20 or over 70 years old.
- Patients who have had radiation treatment in the neck area in the past.
- Patients with a family history of thyroid cancer.
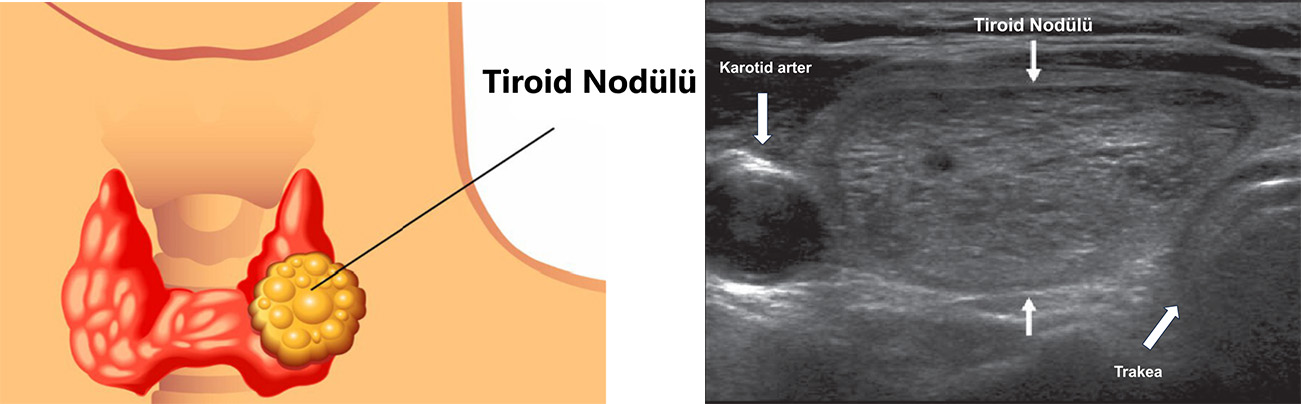
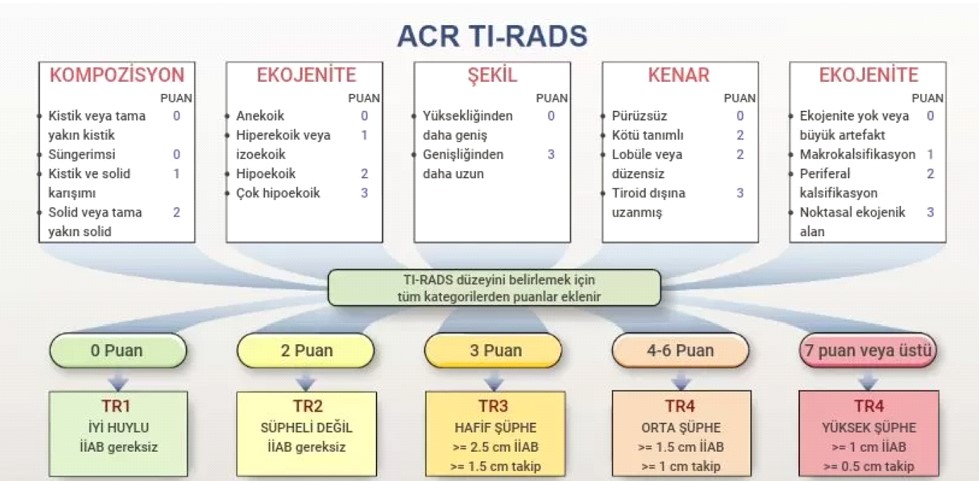
The basic methods for evaluating thyroid nodules include thyroid ultrasound. Thyroid ultrasound plays an important role in assessing nodular thyroid disease. The TIRADS classification is used to indicate the likelihood of a nodule being malignant. Nodules classified as TR3 or above in the TIRADS classification are subjected to fine needle aspiration biopsy under ultrasound guidance.
Thyroid Nodule TIRADS Classification
The Bethesda classification is used to evaluate the fine needle aspiration biopsy results of thyroid nodules.
Bethesda Thyroid Classification
| Bethesda | Biopsy Result | Cancer Risk | Follow-up |
| 1 | Non-diagnostic | - | Repeat biopsy |
| 2 | Benign | % 0-1 | Annual ultrasound follow-up |
| 3 | Indeterminate Atypia | %10-20 | Repeat biopsy Molecular analysis |
| 4 | Follicular Neoplasia | %20-35 | Surgical/Ablation therapy Molecular analysis |
| 5 | Suspicious for Malignancy | %60-80 | Surgical/Ablation therapy |
| 6 | Malignant | %97-100 | Surgical/Ablation therapy |
Bethesda Score 1 (Non-diagnostic):
The biopsy sample taken from the nodule is insufficient for diagnosis. In this case, a second biopsy is recommended.
Bethesda Score 2 (Benign):
The biopsy result indicates that the nodule is benign. In this case, the risk of thyroid cancer is very low (<1%) and regular ultrasound follow-ups are sufficient.
Bethesda Score 3 (Indeterminate Atypia):
In this score, the biopsy result is inconclusive and the risk of malignancy is around 10-20%. In such cases, the biopsy should be repeated, and molecular analysis may help to clarify the diagnosis.
Bethesda Score 4 (Follicular Neoplasia):
The biopsy result suggests a follicular neoplasia. The risk of malignancy is between 20-35%, and surgical removal or thermal ablation therapy is generally recommended.
Bethesda Score 5 (Suspicious for Malignancy):
The biopsy result is suspicious for cancer with a risk of 60-80%. In such cases, surgical removal or thermal ablation therapy is recommended.
Bethesda Score 6 (Malignant):
The biopsy result is conclusive for cancer, with a risk of 97-100%. In such cases, surgery is typically required.
Treatment of Thyroid Nodules
The treatment for thyroid nodules depends on the type of nodule, its size, and whether it is benign or malignant. If the nodule is benign, regular follow-ups with ultrasound are sufficient. However, if it is suspected to be malignant or is causing symptoms, surgical intervention (total or partial thyroidectomy) or percutaneous thermal ablation may be recommended.

 TR
TR